Managing head and spinal injuries
- CareBuddy
- 4 Mins Watch
- 20 Sep 2022
- First Aid & CPR

It’s hard to think of a more important part of our body than our head, primarily because it contains our brain, the operating system of our entire existence! That’s why any injury to the head is a cause for worry. The spinal cord is the highway that connects the brain with every other part of our body, so any spinal injury is equally a cause for concern.
There are 3 major regions of the head that can be injured:
- Scalp (the outermost layer of the head that protects the skull and brain)
- Skull (the bones of the head)
- Brain (the innermost and most protected organ in the head)
Scalp lacerations
These are cuts on the scalp. As the scalp is rich in blood supply, any cut here leads to profuse bleeding. By applying direct pressure, this bleeding can be controlled easily.
Lacerations need to be examined closely for any dents and marks that may indicate a depressed fracture (a fracture where bones have moved inwards).
Skull fractures
These are deeper injuries on the skull below the scalp. Their symptoms include
- Pain, tenderness, swelling and deformity of the skull
- Deep cuts, tears or bruises to the scalp or forehead
- Fluid draining (discharge) from ear or nose
- Unequal pupil size
- Dark purple or blue bruises under the eye due to blood from skull fracture seeping into the soft tissue around the eyes
Brain concussions and compressions
A concussion is a violent jarring of the head (and the brain is shaken) that results in partial loss of consciousness. Its symptoms include
- Partial loss of consciousness
On recovery:
- Headache
- Nausea or vomiting
- Dizziness
- Difficulty remembering events immediately preceding the injury
- Appearing dazed, confused or stunned
A compression is caused by direct force to the head where pressure is exerted on the brain by swelling due to ruptured blood vessels or a blood clot in the skull. Its symptoms include
- A headache which grows in intensity
- High body temperature
- Weakness of one side of the body
- Breathing becomes slow and noisy
- Progressive loss of consciousness
First aid for head injury (skull fracture, concussion and compression)
- Call 995 for emergency medical service
- Keep the care receiver still and make them lie down with the head and shoulders slightly elevated.
- Stop any external bleeding by applying gentle pressure on the wound with gauze pad.
- If there is discharge from the ear or nose, position the care receiver such that the affected ear or nose is lower than the unaffected one. Monitor ABC (airway, breathing and circulation). If care receiver is unresponsive and not breathing, start chest compressions and apply an AED.
- Record and report all observations to the paramedics when they arrive.
Spinal injuries
The spine connects the brain with most other parts of the body through nerves in the spinal cord. That’s why a spinal injury can lead to serious nervous system complications such as paralysis.
Symptoms include
- Tenderness on gently feeling the spine
- Intense back pain
- Paralysis, lack of coordination, or weakness in any part of the body
- Loss of sensation or numbness or tingling of hands, feet, fingers or toes
- Twisted or oddly positioned neck or back
- Difficulty in breathing if the injury is high up the neck
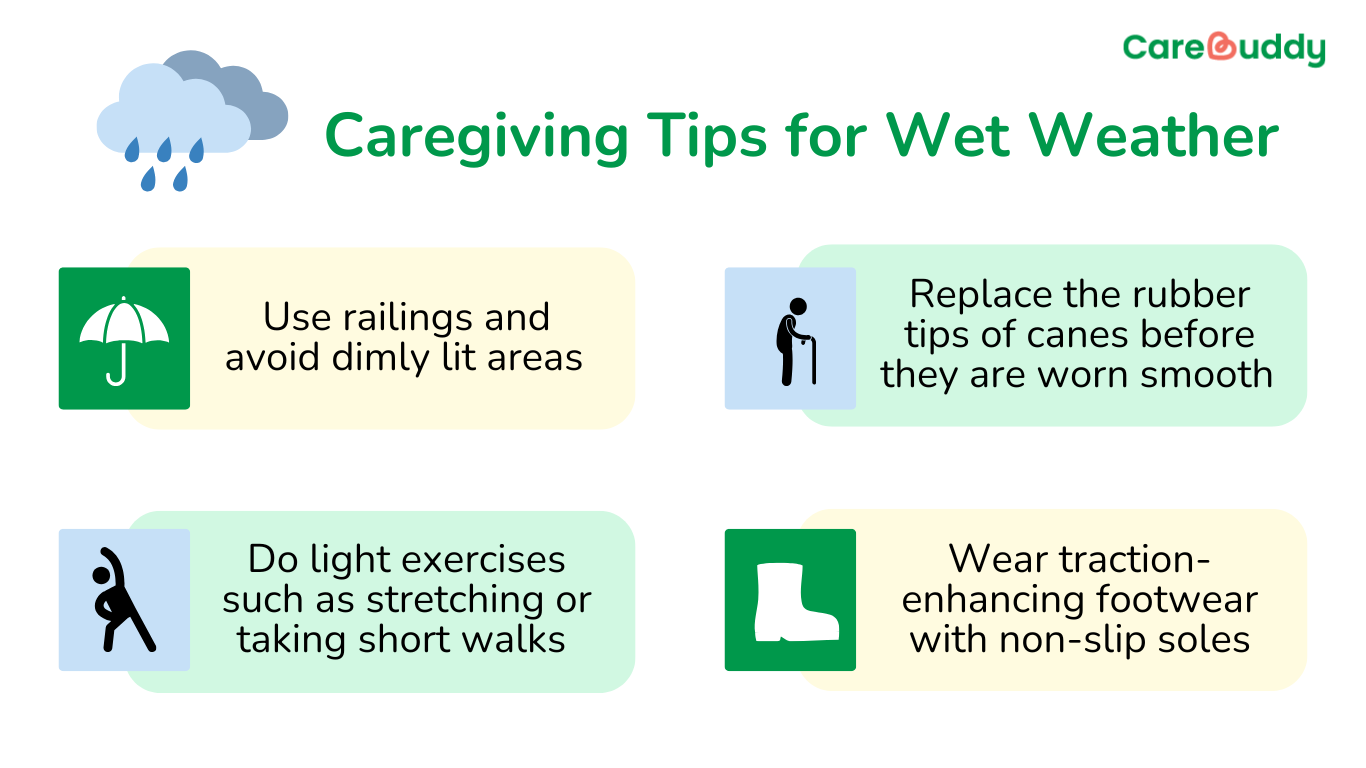
Spinal injuries can be caused by
- Falling from height
- Falling while getting up from a bed or chair
- Falling while climbing up the stairs
- Losing balance while walking with a limb injury such as sprained ankle
- Heavy object falling on the back
- Injury to the head or face
First aid for spinal injuries:
- Call 995 for emergency medical service.
- Reassure the care receiver and tell the care receiver not to move.
- Immobilise and support the head in the position found with objects (e.g. pillows, rolled up blankets or clothing) to prevent further movement.
- Proceed with primary survey (DRSABC as described above) if additional help is available.
- Report details of injury to paramedics when they arrive.
Article reviewed by David Tay, Senior Principal Educator (Nursing and Prehospital Care), HMI Institute.