Observing vital signs in elderly care receivers
- CareBuddy
- 4 Mins Watch
- 19 Sep 2022
- Elderly Care

Older care receivers can experience a wide range of physical conditions. Often, different conditions come together to make things more complicated. This means that caregivers need to be good at observing vital signs and noticing symptoms of various conditions. If anything appears out of order, seek medical support immediately. Early detection is often the difference between life and death, or between a manageable condition and an out-of-control one.
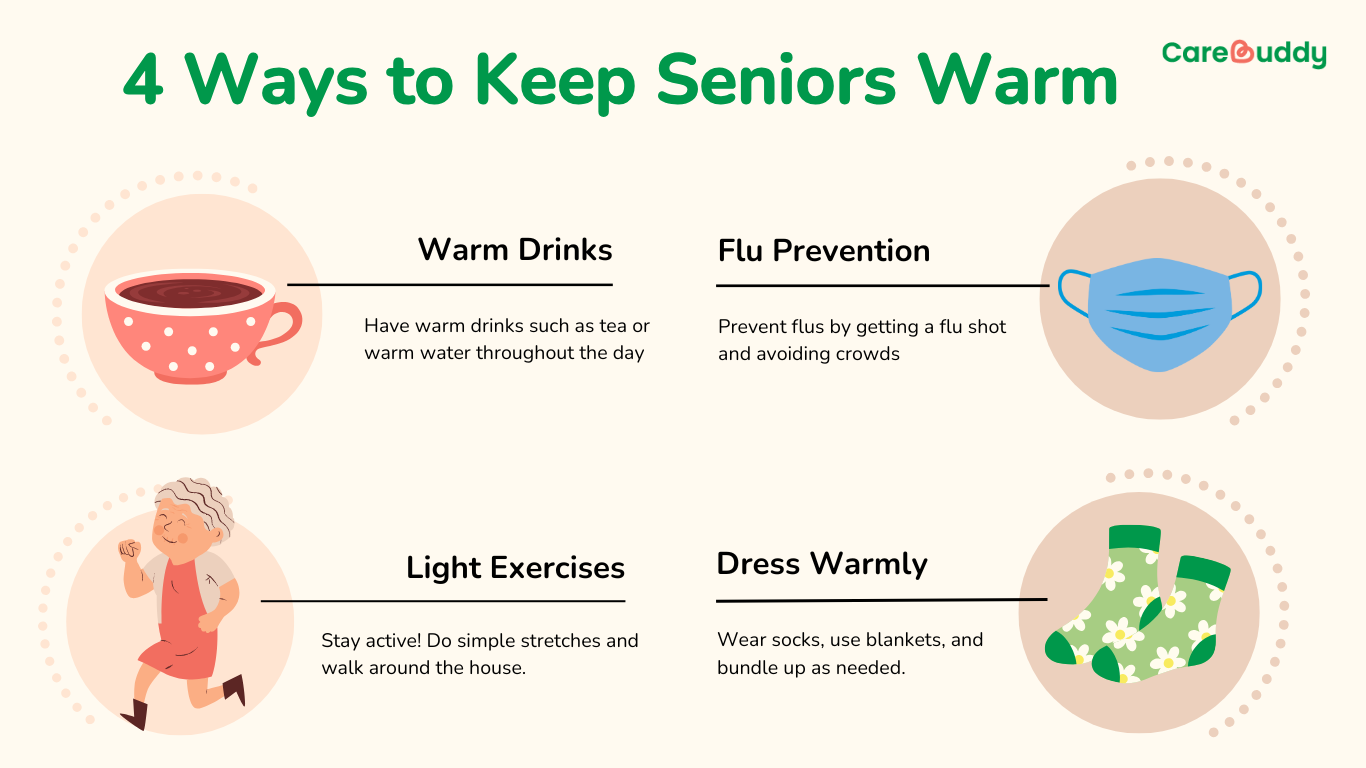
Body temperature
The standard body temperature of most adults is 36.5 to 37°C but the body temperature of the elderly can be lower.
Body temperature needs to be measured when
- The care receiver’s body is hot
- Their face is red
- They feel a chill
- Breathing is difficult
- There’s abdominal pain
Tips for measuring body temperature
- Determine the measurement site (e.g. under the tongue, in the armpit) in advance and stick to the same measurement site as body temperature can be different in different measurement sites.
- Know their usual body temperature so that any change can be quickly noticed.
- If temperature is high, look for other changes such as changes to complexion, expression, heat sensation, increased coughing or complaints.
- Remember that the temperature of an elderly care receiver may not rise even if they have an infection, because the elderly’s response to heat and cold is slow.
Response to temperature changes
- Fever: Report to family members and (if fever is too high) a doctor. If the care receiver complains of heat, cool their body. If they complain of coldness, keep their body warm. Encourage them to drink a lot of water to prevent dehydration.
- Hypothermia: If the care receiver’s hand is pale and cold, assume hypothermia (low body temperature). Protect the care receiver’s body from becoming too cold by keeping it warm through the environment or clothes.
Blood pressure
A blood pressure of 120/80 is considered healthy. It can fluctuate a little, but if it’s too low (e.g. below 100 systolic blood pressure, i.e. the higher number) or too high (e.g. above 150 systolic blood pressure), seek immediate medical support.
Tips for measuring blood pressure
- Measure blood pressure if there’s a rapid change in consciousness or before bathing or exercise.
- Measure in the same site (e.g. right arm) every time and when the care receiver is resting.
- Know their usual blood pressure so that any change can be quickly noticed.
- Check for other changes such as changes to complexion, expression, headaches or complaints.
Response to blood pressure changes
- Place the care receiver at rest and contact medical staff and family members.
- Check if the care receiver is taking any antihypertensive drug (i.e. drugs meant to lower blood pressure)
- If the care receiver’s face turns pale, this could be orthostatic hypotension (low blood pressure due to posture). In this case, get the care receiver to sit or lie back down immediately.
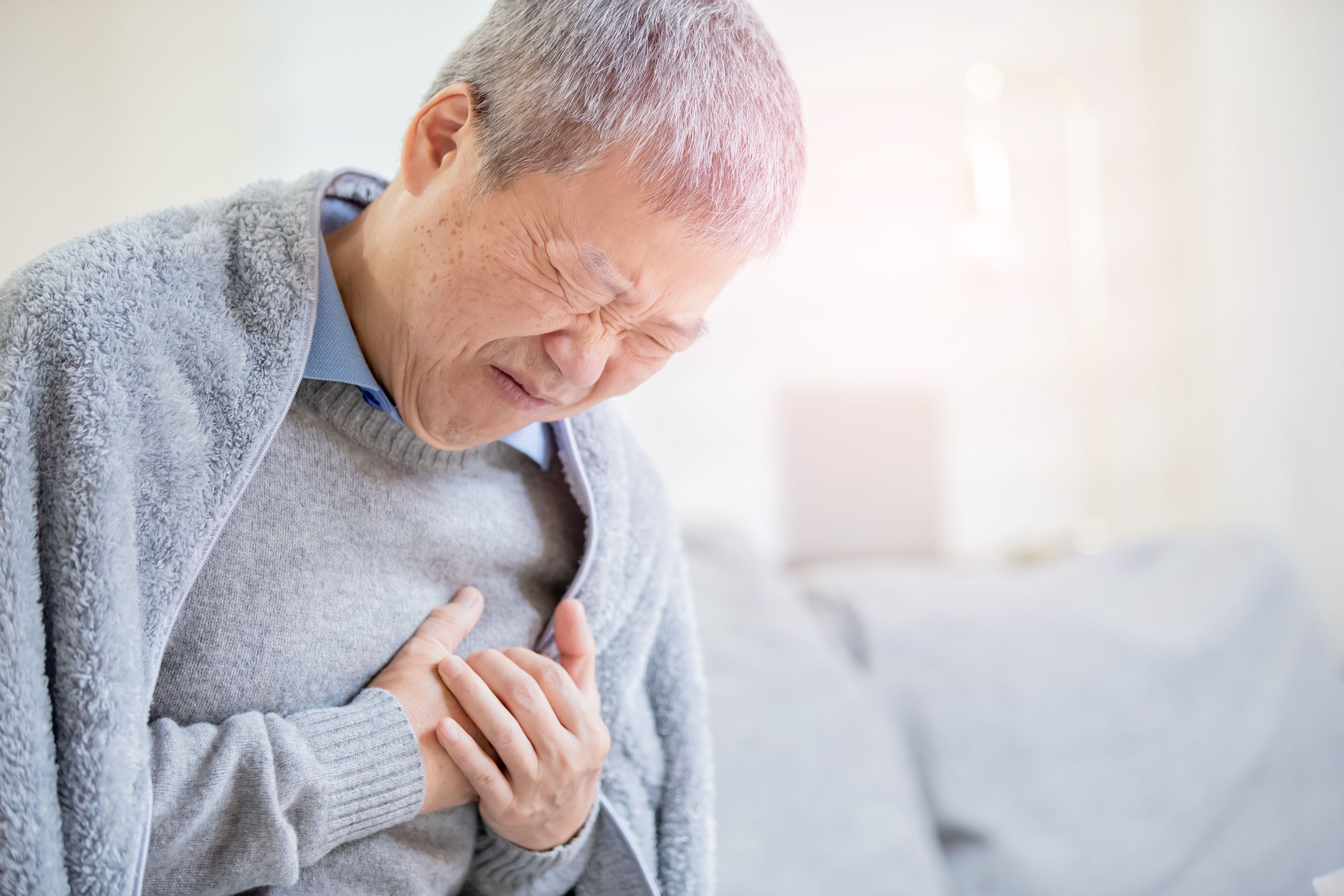
Pulse
The pulse is a reliable measure of the heartbeat. It helps you assess the care receiver’s heart and blood vessels and know states such as stress and fever.
Pulse can be measured on arteries of the wrist.
Tips for monitoring pulse rate
- Place the second and third fingertips on the inside of the wrist at the base of the thumb.
- Press lightly until you feel the pulse. Move to locate the pulse if needed.
- Look at a watch and count the beats in 1 minute.
- Record the pulse rate.
- Watch out for
- Fast pulse (tachycardia)
- Slow pulse (bradycardia)
- Irregular pulse (arrhythmia)
Breathing (respiration)
The state of a care receiver’s breathing helps you know the motion and any abnormality of the lungs or bronchi.
Tips for monitoring breathing rate
- The care receiver is at rest.
- Observe the rise and fall of the care receiver’s chest. One respiration is one complete rise and fall of the chest. Count the respirations in 1 minute.
- Record the breathing rate.
- Also observe the regularity of breathing, breath sounds and breath odours.
- The nostril moving, the lower jaw lowering and shoulders moving are also signs of breathing other than chest rise and fall.
- If the care receiver has a pulse oximeter attached to their finger, this can inform you the level of oxygen in their blood.
If the care receiver has difficulty breathing, let them take a seated posture, then seek immediate medical support.
Consciousness
Assess the care receiver’s state of consciousness using the AVPU scale.
ALERT: Able to tell you their name, place, time of day and what’s happening around them.
VERBAL: Makes some kind of response when you talk to them.
PAIN: Responsive when you inflict pain, e.g. by pressing their shoulders.
UNCONSCIOUS: Not responsive to any of the above.
Call 995 for immediate medical support if the care receiver’s consciousness is low and/or decreasing.
Article reviewed by David Tay, Senior Principal Educator (Nursing and Prehospital Care), HMI Institute.